The Arc was created in the 1950’s out of the wishes and dreams of parents who persisted to create the change they wished to see for their children with intellectual and developmental disabilities (I/DD).
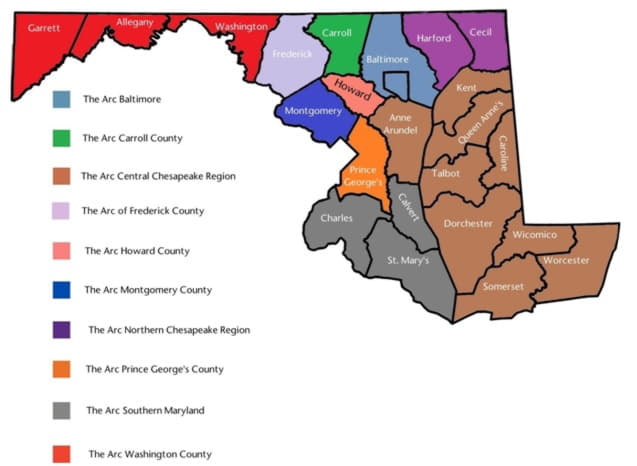
In Maryland, there is one (1) state chapter and ten (10) local organizations who form a network of non-profit providers. The Arc organizations in Maryland collectively support roughly 30% of the people in the state who receive developmental disabilities services. While thousands of people are the direct beneficiaries ofThe Arc organizations’ services and supports, countless others benefit through programs and initiatives, events, trainings, information and referrals, and other family supports.
The Arc organizations offer supports that range from personal care in people’s homes, to coaching in community jobs, daily living skills training, prevocational and day activities, residential services and other health supports for people with disabilities. Of the 10 “full service” Arc organizations, 8 are considered small businesses and all 10 serve as economic engines within their communities, providing jobs, health insurance and other benefits to direct support professionals and others while also supporting people with disabilities and older adults to live and work in their communities, stay healthy, and remain safe.
The Arc organizations across the state recently completed a survey, focusing on the overarching impacts of the pandemic to the organizations, and cost and quality impacts to day-time services for people with I/DD. These services include Community Learning Services (staff supported, small group volunteer work, meaningful community engagement and learning experiences), Supported Employment, Day Habilitation Services, Pre-Employment Supports (internships, apprenticeships, training, and employment discovery), Supported Retirement, Medical Day Services, and Innovative Support Services for Day. Thousands of people throughout the state rely on daytime services and supports in order to work, and they receive varying intensities of staff support. Many families of people with disabilities also rely on these services for their loved ones. Without a caregiver to support their adult child between the typical hours of 8 and 4 p.m., many parents would be unable to hold their own jobs. The importance of these services to our state economy cannot be overstated.
While the numbers reflected in this report are representative of the 10 organizations of The Arc surveyed, we believe the data hasmuch wider applicability, and should be viewed as a sample for what is happening more broadly across the state of Maryland in our Developmental Disabilities Administration-funded Provider Organizations.
As we now enter a period of deep consideration and development of a plan to re-open and recover, the data in this report exposes the true condition of organizations and illuminates considerations our state leaders must have for the rebuilding, stabilization, and future health services for people with intellectual and developmental disabilities. DDA provider organizations ultimately do the work of the state; supporting over 17,000 people with I/DD in a variety of community settings and the state has a responsibility to ensure the safety, quality, and viability of our system.
Overarching Considerations:The COVID-19 pandemic has created unprecedented and unique challenges for DDA organizations in the state. Some of these organizations indicate they may not survive the pandemic without intervention from the state through funding and policy changes; to help shore up what has been disrupted. If left unaddressed, or worse, if budget cuts are instituted for the more than 200 DDA organizations in the state (including the 10 Arc organizations surveyed in this report), we fear there will not be enough providers or services to meet the needs of people with I/DD.
Provider business failures were rare occurrences in apre-pandemic Maryland. In the past, when provider businesses failed, it was historically the larger organizations (The Arc and others) that had the infrastructure and reserves to assume the clientele, workforce, and debt of the failing organization. Now, most organizations report they have little left in reserves and with excessive pandemic-related costs, revenue shortfalls, political uncertainty, and resultant “risk aversion”,it is unlikely they would be able to step in if something went wrong with another organization. Even the large organizations are not immune from the ravages of the pandemic. What will happen if one of them finds they do not have the resources to operate?Our safety net has been compromised and those organizations who are able to find a way to survive are expected to curtail their services, leaving thousands of men, women and children with disabilities and their parents without basic, needed services and supports.
Survey Participants: All ten of The Arc provider organizations in the state participated in the survey, who provide direct services and supports to 5453 people with intellectual and developmental disabilities and thousands more family members, children, and adults with disabilities who receive direct services from these organizations but do not have DDA funding for day and employment, residential, camps, family support classes and trainings, respite services, Information and referral services and other supports.
The combined workforce of The Arc organizations exceeds 4000 employees. Of this number, 88% are front line workers, primarily known as Direct Support Professionals. The service area of The Arc organizations spans from the western border of Garrett County to the northern point of Cecil, and from the southern tip of St Mary’s County to the eastern end of Worcester County. All 24 Maryland counties, and Baltimore City, are supported by The Arc either through direct services, or though our many supportive advocacy and educational opportunities.
Survey Findings
Added Expenses:There have been significant increases in many of the costs of doing business.
Categories of added costs include:

Personal Protective Equipment (PPE) and additional cleaning supplies:While the Developmental Disabilities Administration provided two “rounds” of PPE to organizations throughout the state, the PPE was enough to cover only a fraction of the need for roughly half of the existing providers in the state. A couple of The Arc organizations have not had anypositive cases of COVID to date however, according to the survey, their costs for PPE and additional cleaning supplies ranged from $7,500 to $20,000. Most of The Arc organizations have had at least one positive case of COVID, with three chapters experiencing multiple outbreaks of COVID-19. PPE and cleaning supply costs for those organizations ranged from $25,000 to $250,000 over a period of two months. The total cost of PPE and additional cleaning supplies from mid-March to mid-May was $409,675 for all 10 organizations.

Increased Salary and Pay-Related Expenses: All of The Arc organizations found they needed to institute periods of incentive and hazard pay for their front-line workers. This was necessary to properly compensate Direct Support Professionals working in high-risk health environments such as small congregate group home settings. As the state of Maryland prioritized PPE for hospitals and nursing homes, disability support organizations initially could not obtain even basic PPE. Conditions have improved slightly, however The Arc organizations continue to struggle to obtain basic PPE such as hospital masks, gloves, and face shields. Items such as disposable gowns, N95 masks, and shoe coverings are still very difficult to obtain and if they were available, they may be purchased at high costs and only in limited supplies.
In total, The Arc organizations paid increased overtime, incentive pay, hazard pay, and sick leave benefits costing $1.88 Million in a two-month period. The range was $72,500 to $750,000 spent per organization on enhanced compensation and leave benefits during this period.
Decreased Revenues:The Governor ordered adult day programs to be closed on March 19[i]. Many individuals with intellectual and developmental disabilities and their Direct Support Staff were suddenly faced with a unique challenge; how to continue to provide critical support with no building or community place in which to provide it.

While some individuals with I/DD remained supported during the day within their residential group homes, other individuals (who did not have DDA funding approval for both residential and day service supports) were suddenly remaining home with their families, with no paid support (or limited paid support) as parents of advanced age and pre-existing conditions feared exposure of COVID through allowing paid caregivers into their homes.
Providers of day services were severely hampered, given the current service and setting definitions for Medicaid payment, community closures and stay-at-home orders,and most lost tens of thousands of dollars in revenue as they struggled to keep their direct support workforce employed, with little to no ability to generate offsetting revenues for their continuing, and growing, operational expenses.
Some of The Arc organizations were eligible for the federal COVID-19 emergency Paycheck Protection Program (PPP) loans from the Small Business Administration. These loans (which may be forgiven in part or in whole) provided funding to offset payroll and operating expenses for a period of up to 8 weeks. The organizations who obtained the PPP used the funding to help maintain their workforce and operations, despite the substantial DDA revenue losses the organizations sustained. The larger organizations of The Arc were not eligible for the PPP program and faced more severe financial consequencesduring this period.
While some flexibility was eventually created with an emergency amendment to the state’s Home and Community Based Services (HCBS) Medicaid Waiver (also known as the Appendix K), that waiver amendment was not approved until a full month into the pandemic. Changes to billable service definitions created some opportunities for providers to bill for services in different settings for different units of time, and remote services were approved at one point which allowed individuals with disabilities to receive telehealth supports.
Many individuals have been able to resumeneededservices through remote/tele supportand other flexibility in service definitions included in the Appendix K. Many are thriving with this new way of receiving support, however, there remains a larger segment of the population for whom remote services are not a viable alternative to in-person support.

Barriers to Participation in Remote Supports
The reasons provided, to explain the barriers to participation in remote/tele supports, fell into 4 overlapping “buckets”. For those individuals with I/DD who have been unable to participate in remote supports:
63% of The Arc providers reported the cases are related to a lack of technology. Individuals and their families either did not have the needed technology or lacked the skills to properly utilize the technology needed to meaningfully access tele support;
50%of the them alsoreported an inability to access tele support due to a lack of “service”. Either they lived in remote areas of the state or the inner city within a service “dead zone”, or they did not have the financial resources to purchase internet service. Internet service is not a service that is currently funded by the DDA at this time. Some families do not even have a telephone through which a provider could provide assistance;
75%of the providers reported that in many cases, the individual’s disability was preventing the person from meaningfully participatingin remote services; and
All 10 (100%) of The Arc providers reported that the lack of participation of many people was due in part to disinterest in receiving remote services. Families reported that they need in-person assistance and caregiving for their loved oneand tele support was simply not a service that would effectively replace staff and fulfill their needs.Some individuals disinterested in receiving remote services also stated they were not interested in being on the phone or computer as they truly needed the physical assistance from their Direct Support Professional. There were also some reports by some as amistrust in technology or fear that they would be watched, hacked, or otherwise harmed by using technology. For many, there was a general disinterest in being on the phone or in front of a computer for any great length of time, even just 1 hour per day to allow the provider to bill for the remote service.
The average attendance rate, each month across all day service options and all organizations of The Arc was 83.37% prior to March 2020
Since the pandemic hit, the average attendance rate in the two-month measurement period for this survey (April and May) across all day service options and organizations of The Arc was 40.06%.This calculation includes individuals who utilized tele supports during this period.
The data shows a decline in service utilization of almost 52% since the start of the pandemic.
With an inability to support people at full capacity, continuing costs to maintain the business to satisfy service provision needs and state documentation requirements, the effort to maintain the critical DSP workforce, and tens of thousands in un-reimbursable health-related expenses,the revenues lost, across The Arc organizations,($1.785 million in April and an additional $2.079 million in May) totaled more than $3.8 million.
Upon further analysis of the data, the increase in losses between April and May is primarily due to the depletion of state-payable “bed-hold” days for the year, otherwise known as “retainer” days.

Of consideration, most of The Arc organizations have maintained their workforce, somewhat due to relief provided by federal PPP loans, but report they may need to consider future furloughs of workforce or layoffs if conditions, including relief funding from the state, don’t improve.
One organization reported that although they maintained the employment of 100% of their workforce, they still received 70 claims for unemployment benefits which include the Families First Coronavirus Response Act additional benefit amount of $600 per week.
Another organization noted that they had been aggressive with admissions over the past several years, pre-pandemic, to expand services to those in need. This has come to a halt with the pandemic. A Manager for the organization reported having over 50 people with disabilities “in the pipeline” prior to COVID-19, with about 20 people (not including Transitioning Youth) who were in the process of being brought into services in the Spring. These admissions are now on hold due to financial uncertainty and the pandemic. The ripple of this will affect not only the individuals with I/DD but their families and the state’s economy, if parents are not able to work due to a responsibility to care for their adult children during the day.

The Future: A Plan for Recovery and Sustainability
It is clear we are living in a new world. While many things will return to pre-pandemic states over time, there are many things that are permanently altered.
Prior to the pandemic, there was a movement for developmental disabilities services and supports to be completely in and of the community. The movement away from large group homes and sheltered workshops has been viewed as an extremely positive development over the past few years, propelled by the CMS “Final Rule” requirements for states to receive continued HCBS Medicaid funding. DDA services had been provided in smaller groupings of people, formed according to individual interests and needs for support, but still dictated by “group funding” formulas and levels. Funding has historically been predicated on, and allocated to, Day services providers for groupings of 4 to 8 individuals, with meaningful day time services provided to people in close proximity to one another. Staffing for these groupings varied but were typically with 1 to 2 Direct Support Professionals who assisted individuals to participate in community activities, educational and recreational experiences, group volunteerism or group work. Transportation services varied as well but were usually provided for groups of 5 to 11 people who were picked up at their homes in the morning, according to a predetermined route, andtransported to a common location to start and end each day.
With CDC recommendations to limit group sizes, expand distances of proximity, expand cleaning protocols, and place additional consideration and care on the needs of people with underlying health conditions and advanced age, everything must be re-examined.
We will need to re-design services, considering one person at a time; their interests and needs. Groupings of individuals with I/DD and their Direct Support Professionals will need to be smaller. Transportation may need to be less congregate and maybe even provided individually. People with underlying health conditions and advanced age may not be advised to venture out of the house for several months, or until there is a vaccine for COVID-19.
In addition, there is a segment of the population of people with disabilities who cannot tolerate wearing a mask. They may experience extreme discomfort and feelings of asphyxiation wearing a mask, due to a heightened sensory condition, or may be unable to wear a mask because of a medical condition in which their airway cannot be obstructed, even by a sheet of fabric. These individualsalso present additional considerations as we look to the future: how do we keep them safe and healthy and how will we keep their caregivers, the community, and their families safe from possible exposure?
What we have learned and should apply to our planning for services and supports in our new world:
It is going to take time and re-consideration of the needs of each person and families who are supported by DDA. People with developmental disabilities, once funded for support in groups, may need additional funding as we move to individual supports or at minimum, smaller groupings.
This will require an expansion of the workforce. Prior to the pandemic, it is well documented that DDA funding was insufficient to compensate DSPS at little more than minimum wage. DSP turnover across agencies was between 40 and 50% per year with almost half of the DSPs exiting within the first 6 months of employment. The hours were long, and the work intense. The position required skill, patience, organization and compassion.
Now, the job requires even more; DSPs have been on the front lines of this pandemic since its beginning. They put themselves at risk every day as they work to support fellow Marylanders with developmental disabilities. Supporting individuals individually or in smaller groupings will require higher autonomy and decision-making ability of DSPs. DSPs who were once able to rely on the guidance and support of other DSPs in their small groupingsmay now and forever more be working alone with one or more individuals.
Transportation, as we knew it, may not ever be the same again.
While we embrace this development, as it moves us further away from the days of institutional services, it will be more costly. As recognized by the DDA, the funding component for transportation was already inadequate prior to the pandemic. The new rates that were developed (but were not included in the Governor’s FY21 budget), would have increased the pre-pandemic transportation services rate components significantly. Group transportation is always less costly than individual trips, and our movement away from high density transportation services will cost much more as developmental disabilities providers re-open.
Cleaning services (time to clean, supplies needed) and protocols must be upheld as we recover. Providers will continue to need PPE for the foreseeable future.
Cleaning time, cleaning supplies and PPE are not currently reimbursed by the Developmental Disabilities Administration in fundedrates. As these necessities carry heavy price tags, and none of the costs of services or supplies may be passed on to the people with I/DD who are supported due to Medicaid rules, state funding is needed for PPE, cleaning supplies, and the time to clean now, and into the future.

Recommendations to Ensure Health of Participants, Quality Provider Services and to Enable to Recovery of Developmental Disabilities Services Across Maryland
• Designate and treat Direct Support Professionals as Essential Healthcare Workers.
Our state has designated home and community-based providers as essential health care workers, but funding has not been enhanced to provide incentive and hazard pay for working in potentially dangerous environments, nor has PPE been prioritized for Direct Support Professionals. Hazzard pay is only reimbursed by DDA at a rate of time and a half for Direct Support Professionals working directly with someone who is presumed or confirmed positive for COVID. This is in stark contrast to the pay provided to other essential workers in Maryland, many of whom for which the state has funded enhanced pay during this period in recognition of the additional risks of working in a highly vulnerable environment, and without the requirement they be working directly with a person who is positive for COVID before the enhanced pay is provided. It is time to recognize DSPs with pay that is commensurate with their levels of responsibility, training, competencies, risks, and autonomy. This will only be possible with increases to DDA funding to support the pay increases and pay-related expenses for DSPs.
We also ask our state leadership to prioritize PPE for Direct Support Professionals as they work in small congregate settings, and often with individuals who may have an inability to exercise prior handwashing and cough-covering, and social distancing, placing all at advanced risk of illness.
In addition, Maryland is receiving relief funding through the Coronavirus Aid, Relief, and Economic Security (CARES) Act. According to KFF (see footnote), Maryland has received at least$742,225,306 in the first disbursement of the CARES Act Payments.[i]
Division B of the CARES Act provided among other things $100 billion nationally to reimburse hospitals and other health care entities responding to coronavirus for health care-related expenses or lost revenues that are attributable to coronavirus.[ii]
In our neighboring state of Pennsylvania, the Senate recently took action to approve the allocation of an $260 million of their federal CARES funding for providers of intellectual disability and autism services for critical needs created by the COVID pandemic.[iii]
If Maryland has received CARES Act funding under Division B, we ask that a portion be devoted to relief for our DDA providers as an eligible “health care entity”, in reimbursement for expenses incurred responding to the coronavirus, health care-related expenses, and lost revenues attributed to coronavirus.
We must also recognize that there will be a segment of the population of people with I/DD who are of advanced age and how have pre-existing conditions which would make them highly vulnerable to serious effects of COVID-19, and others who, because of their conditions, have an intolerance to wearing masks or any other protective equipment. They will likely need to be phased back into their day and residential supports later than others and the costs of converting them from their previous small group supports to a 1:1 support will be more costly. There must be a mechanism for accessing funding support to address these situations fairly and effectively.
In addition, billable services and supports should allow for reimbursement for additional cleaning supplies and time to clean, and for additional costs of smaller transportation arrangements. This will be necessary to keep people with developmental disabilities and staff safe and healthy now and into the foreseeable future.
The Arc organizations collectively offer our ideas and commit our administrative time and support to this shared purpose; the development of our post-crisis framework for developmental disabilities services and supports in Maryland.
For any questions related to the contents of this report, please contact Ande Kolp, Executive Director of The Arc Maryland.
Contact:
email: akolp@thearcmd.org
phone: 443-851-9351
website: www.thearcmd.org
[i]KFF Analysis: Number of Coronavirus Cases, Distribution of $30B in CARES Act funding and Medicare Advantage Penetration by State (kff.org)
[ii]KFF: The Coronavirus Aid, Relief, and Economic Security Act: Summary of Key Health Provisions (kff.org)
[iii]https://www.pasenategop.com/blog/senate-republican-leadership-passage-of-budget-cares-funding-sets-course-for-recovery/
[iv]https://www.ancor.org/sites/default/files/impact_of_covid-19_on_organizations_serving_individuals_with_idd.pdf